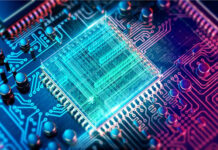
Biomedical engineers are researching technological advancement related to the medical field to make the treatments of various ailments more successful and robust. It sets virtual reality to revolutionize healthcare by allowing the medical practitioners to reach deep into the human body to model the mechanisms in the individual bodies to tailor the treatments. Researchers are working to develop tools using virtual reality to allow medical practitioners to gain fundamental knowledge about the surgical outcomes beforehand. This means to stimulate the human body functions before and after the perceived surgical intervention to find the best possible solution.
Heart disease is the number one cause of death in many regions of the world, including the USA. Therefore, extensive research is being conducted throughout the medical and biomedical world to improvise treatments in the cardiovascular field. The advancements in the biomedical engineering field especially virtual reality have produced several tools, interventions, and investigative laboratory tests to better diagnose and treat cardiovascular disease. One of these tools is a 3D VR blood flow simulator.
Biomedical experts at the Duke University aim to develop a massive 3D VR fluid dynamic simulator for modeling the blood flow mechanism in the full human arterial system at the sub-cellular resolution. The basic aim of the 3D VR blood flow simulator is to introduce a higher level of accuracy in the prediction of surgical outcomes. Cardiovascular surgeries for geometric alterations to blood flow like stent placement, conduit insertions, and other solutions are significant in the treatment of various heart problems. The ability to accurately simulate the patient’s specific vasculature variables is a great technological advancement in 3D VR for cardiovascular care. It allows medical practitioners to make the most accurate decisions in terms of medical interventions tailored for every individual patient.
The 3D VR blood flow simulator is not only substantial support for the doctors and surgeons but also the patients. VR technology allows the patient to be taken through their anatomy and pathology to better understand the treatment being provided to them.
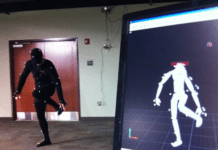
This 3D VR dynamic blood flow simulator is called HARVEY. Though the simulator is ready to use, the principal obstacle according to the Duke University researchers is the user interface. There is virtually no use for the tool if the practitioners are not comfortable using it. HARVEY required the knowledge of C computer language coding and command-line interfaces. This limitation meant the usage of the simulator was hurdled by the difficulty of operation.
Amanda Randles, the Alfred Winborne and Victoria Stover Mordecai Assistant Professor of Biomedical Sciences at Duke, has introduced the graphical user interface for the HARVEY simulator called Harvis. Graphical user interface means that everybody with basic knowledge of a keyboard and mouse can use the 3D VR blood flow simulator with essential training.
Once the user interface provided for the HARVEY is accepted by the medical practitioners and comes into wide use. The cardiovascular surgeries will advance by leaps. The surgical team will be able to plan the treatments using a more intuitive 3D virtual reality interface. They will perceive the outcome of different placements of stents to assess the efficiency and will choose the best outcome. Amanda Randles also foresees the use of these types of 3D VR tools in biomedical research in the personalized flow space.
In the recent study, Amanda Randles and her aides, research associate Harvey Shi and graduate student Jeff Ames, demonstrate the use of GUI Harvis. The real-time testing involved medical students and biomedical researchers. They were asked to simulate three unique situations.
Placing a conduit between two blood vessels
Expanding or shrinking the size of a blood vessel
Placing a stent within a blood vessel.
The test users were given three choices for the user interface, i.e.
Standard mouse and computer screen
A “Z-space” semi-immersive virtual reality device, a special pointing tool combined with a monitor and 3D glasses.
HTC Vive display device for fully immersive virtual reality experience.
The result showed that standard mouse and computer screens, as well as the 3D virtual reality experience, were very well received by the test users. They did not feel comfortable with the semi-immersive virtual reality device because of the unique controls and hardware.
The study used both the most and least immersive interfaces but did not find any major difference in quality and efficiency. However, Randles noticed a difference in the user’s reactions. According to her;
“People enjoyed the 3D VR interface more and if they enjoyed it more, they’re more likely to use it. It could also be a fun and exciting way to get students engaged in classes about the vasculature system and hemodynamics.”
Randles has more research plans based on this revolutionary 3D Virtual Reality blood flow simulator, Harvey. She now wants to investigate if a 3D blood flow interface can help medical students. The idea is to find out if this interface can help the students keep principal knowledge better than the traditional form of studies. If proved, this can be a landmark achievement in the field of medicine and education. It will allow the students to have a more intensive and broad knowledge base, eventually improving the quality of treatment imparted to patients.
The development of the graphical user interface and virtual reality experience for the simulation of cardiovascular blood flow is a landmark revolution in the field of medicine. Once it comes widely in practice, it opens doors for many other medical treatments to adopt the same model.
References:
Harvey Shi, Jeff Ames, Amanda Randles. Harvis: an interactive virtual reality tool for hemodynamic modification and simulation. Journal of Computational Science, 2020; 101091 DOI: 10.1016/j.jocs.2020.101091
www.sciencedaily.com/releases/2020/05/200513135519.htm
Duke University. “3D VR blood flow to improve cardiovascular care: 3D interface provides cellular-level, full-body blood flow modeling to study and treat cardiovascular disease.” ScienceDaily. ScienceDaily, 13 May 2020.